Reduced blood pressure = reduced performance?
- DNA_Rower
- 1k Poster
- Posts: 160
- Joined: October 16th, 2011, 7:08 pm
- Location: Berlin, Germany
- Contact:
Reduced blood pressure = reduced performance?
I've been trying to get my blood pressure under control for for a year now.
Increasing dose of 1st line treatment (Ramipril) didn't work, adding another medicine didn't work. I just switched to some other triple-drug combo, and suddenly my BP is now in a optimal/normal range.
To give you an idea I would previously get 140-160 / 90-110. Tonight I got 111/61 (measured a few hours after erg session) and I'm now usually 12X/7X, which is a pretty good reading.
However I notice that as soon as I switched medicine my performance on the erg has dropped. I've been following the Pete Plan for a while and I've always managed to improve scores on the 3 week cycle. Now - I have lots loads of stamina. It is a bit warmer in the gym now (and I hate that!), since Berlin has warmed up so I initially blamed the temperature increase.
I have to go back to the doc to report improved BP anyway, but I'm wondering if this is a "side-effect".
Anyone else had similar experience?
OK elsewhere lots of other people have had lower stamina once taking BP drugs (when they work). The physiology is kinda obvious, but I'd still be interested if anyone has experience of this. e.g. https://www.healthboards.com/boards/hig ... amina.html
Increasing dose of 1st line treatment (Ramipril) didn't work, adding another medicine didn't work. I just switched to some other triple-drug combo, and suddenly my BP is now in a optimal/normal range.
To give you an idea I would previously get 140-160 / 90-110. Tonight I got 111/61 (measured a few hours after erg session) and I'm now usually 12X/7X, which is a pretty good reading.
However I notice that as soon as I switched medicine my performance on the erg has dropped. I've been following the Pete Plan for a while and I've always managed to improve scores on the 3 week cycle. Now - I have lots loads of stamina. It is a bit warmer in the gym now (and I hate that!), since Berlin has warmed up so I initially blamed the temperature increase.
I have to go back to the doc to report improved BP anyway, but I'm wondering if this is a "side-effect".
Anyone else had similar experience?
OK elsewhere lots of other people have had lower stamina once taking BP drugs (when they work). The physiology is kinda obvious, but I'd still be interested if anyone has experience of this. e.g. https://www.healthboards.com/boards/hig ... amina.html
A: 40; H: 184cm; W: 76kg.
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
- hjs
- Marathon Poster
- Posts: 10076
- Joined: March 16th, 2006, 3:18 pm
- Location: Amstelveen the netherlands
Re: Reduced blood pressure = reduced performance?
38 and you take bloodpressure medice  sounds bizar to me.
sounds bizar to me.
- DNA_Rower
- 1k Poster
- Posts: 160
- Joined: October 16th, 2011, 7:08 pm
- Location: Berlin, Germany
- Contact:
Re: Reduced blood pressure = reduced performance?
It's not "bizarre" mate, just unusual.hjs wrote:38 and you take bloodpressure medicesounds bizar to me.
I'm 38, good weight, reasonable diet, and pretty fit... but I have a family history of high Blood Pressure and one dodgy kidney.
Scottish genetics are not the best...
A: 40; H: 184cm; W: 76kg.
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
- hjs
- Marathon Poster
- Posts: 10076
- Joined: March 16th, 2006, 3:18 pm
- Location: Amstelveen the netherlands
Re: Reduced blood pressure = reduced performance?
It is, you really should look at your lifestyle/eating.DNA_Rower wrote:It's not "bizarre" mate, just unusual.hjs wrote:38 and you take bloodpressure medicesounds bizar to me.
I'm 38, good weight, reasonable diet, and pretty fit... but I have a family history of high Blood Pressure and one dodgy kidney.
Scottish genetics are not the best...
Family history is often family lifestyle.
From a distance ofcourse but still find it very very odd. And meds often reduce the pumping meganism of the heart, so your "fitness" will be limited.
My take is to improve your health, high blood pressure is a matter of inflexible veins, already at this age....
Re: Reduced blood pressure = reduced performance?
Yes, OP should definitely cut down on the deep fried Mars bars and pizzas.  (joke)
(joke)
Seriously though, I've no real knowledge of BP and meds, but has the OP experimented with nitrate supplementation eg. via beetroot juice or L-citrulline, as a way to manipulate BP?? Just a thought.
Seriously though, I've no real knowledge of BP and meds, but has the OP experimented with nitrate supplementation eg. via beetroot juice or L-citrulline, as a way to manipulate BP?? Just a thought.
Paul, 49M, 5'11" 83kg (sprint PBs HWT), ex biker now lifting
Deadlift=190kg, LP=1:15, 100m=15.7s, 1min=350m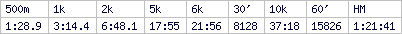
Targets: 14s (100m), 355m+ 1min, 1:27(500m), 3:11(1K)
Erg on!
Deadlift=190kg, LP=1:15, 100m=15.7s, 1min=350m
Targets: 14s (100m), 355m+ 1min, 1:27(500m), 3:11(1K)
Erg on!
- NavigationHazard
- 10k Poster
- Posts: 1789
- Joined: March 16th, 2006, 1:11 pm
- Location: Wroclaw, Poland
Re: Reduced blood pressure = reduced performance?
Much depends on exactly what BP drug(s) are being taken, when and in what quantities, in conjunction with all the other myriad factors that can affect blood pressure. Different people react differently to different regimens, in short, and things like hydration levels, stress, sodium levels in the diet, hormonal cycles, other drugs like (say) advil that can affect BP, sleep cycles, time of day, biological sex, etc. etc. complicate matters considerably.
This includes the way your BP's being read -- you need to be sure you're actually getting accurate readings over time that reflect any underlying pathology that might be there...
This includes the way your BP's being read -- you need to be sure you're actually getting accurate readings over time that reflect any underlying pathology that might be there...
67 MH 6' 6"
-
David Pomerantz
- 1k Poster
- Posts: 111
- Joined: July 18th, 2010, 2:33 pm
Re: Reduced blood pressure = reduced performance?
I was on a BP med for a short time and remember thinking my erg performance declined as well. The beta blockers decrease both heart rate and force of contraction, so perhaps if you are taking one of those that explains the erg.
Here’s some good news though. I’m a doc, and have never really believed I could alter my BP with changes in weight or diet. Boy was I wrong. I’ve found that very small changes in weight can have big effect on BP. I’ve gone from using meds to not needing them simply by cranking up the rowing.
Dave
Here’s some good news though. I’m a doc, and have never really believed I could alter my BP with changes in weight or diet. Boy was I wrong. I’ve found that very small changes in weight can have big effect on BP. I’ve gone from using meds to not needing them simply by cranking up the rowing.
Dave
- NavigationHazard
- 10k Poster
- Posts: 1789
- Joined: March 16th, 2006, 1:11 pm
- Location: Wroclaw, Poland
Re: Reduced blood pressure = reduced performance?
Cheers Dave, I thought your name was familiar in this context. With a bit of sleuthing I figured it out.
The OP might want to look at this thread from 2013: viewtopic.php?f=4&t=13740&p=189694&hili ... en#p189694
My contribution at the time was this:
Oh, the OP should take heart (pun intended) that both Dr. Dave and myself are still plugging away at it. I'm the current British and World age-group title holder for 2k, for example, despite medical problems on a whole new front (anti inflammatory-induced diabetes). And my BP was 123/67 this morning after my coffee, with a pulse rate of 53.....
The OP might want to look at this thread from 2013: viewtopic.php?f=4&t=13740&p=189694&hili ... en#p189694
My contribution at the time was this:
Unfortunately the UK Forum and the associated blogs have since gone defunct, and I don't really have much saved from those days except logbook results that mostly track meters rowed in workouts. There >might< be something floating around this Forum in one of the old USIRT threads, but if there is I can't find it using the Forum search function. I can say that I was 6:18.8 in my time trial to make the squad, on 10/28/07, and I vaguely recollect producing something on the order of 6:30 six weeks later at the EIRC. Some of the performance dropoff had to have been psychological, i.e. an understandable reluctance to push hard enough to rather literally kill myself. But as I now recall the episode, most of it would have been a genuine function of the medication. Considering that there are several widely circulated studies suggesting that ACE inhibitors don't normally impact endurance/performance much, if at all, I'd say the experience shows how idiosyncratic any given athlete's response to them can actually be.Cheers David, just now catching up to this. Back in 2007, as a 50s HW, I'd qualified for the C2-sponsored US Indoor Rowing team with a time trial 2k around 6:20 and was probably in 6:12-6:14 form. We were to compete in the European Championships in Dresden that year. The organizers required a prior, routine medical screening for competitors. Mine revealed significantly elevated blood pressure -- a shock to everyone, especially me. I was 100% sure it was either a spurious reading or else an artifact of some ridiculously difficult interval workout. However the doctors would not clear me for competition without starting me on an ACE inhibitor. I had about a week or two to get used to it before the competition. In my opinion it dramatically inhibited both my pre-race sharpening and also my performance (somehow I managed a bronze). You might find some utility in reading through my blog on the UK Forum from that period. See for example http://concept2.co.uk/forum/blog.php?b=38354 (you may have to register for the Forum to get access). For what it's worth, I went off the medication in 2008 and the problem -- if there ever had actually been one -- has not recurred. I did invest in an electronic home BP gauge and do test myself periodically, just to make sure.
Oh, the OP should take heart (pun intended) that both Dr. Dave and myself are still plugging away at it. I'm the current British and World age-group title holder for 2k, for example, despite medical problems on a whole new front (anti inflammatory-induced diabetes). And my BP was 123/67 this morning after my coffee, with a pulse rate of 53.....
67 MH 6' 6"
-
lindsayh
- Half Marathon Poster
- Posts: 3635
- Joined: June 23rd, 2013, 3:32 am
- Location: Sydney, Australia
Re: Reduced blood pressure = reduced performance?
I'm always nervous about anecdotal medical discussions on non medical forums but......FWIW
Many hypertension "sufferers" have no other medical problems and the condition is described as "essential" or idiopathic and is probably genetic. My diagnosis was about 5 years ago persistent 150+/90ish monitored a lot for 6 months in spite of serious levels of fitness for 30 years and no other life style risk factors. My dad "gave" it to me as a present (along with the OA in my knees!) There was no way of increasing exercise or changing diet in any significant way. Started treatment with Telmisartan (Micardis) which is an ARB (Angiotensin Receptor blocker) rather than an ACE inhibitor. Since treatment have been continuously 120/80 and all my PBs have been set since treatment started so no negative effect at all.
Interestingly I discovered tonite that there is a secondary effect on muscle that in fact may be beneficial to exercise and has been suggested as a metabolism modifier that has some interest via WADA (though isn't on any lists). https://insights.ovid.com/crossref?an=0 ... 3000-00002
Many hypertension "sufferers" have no other medical problems and the condition is described as "essential" or idiopathic and is probably genetic. My diagnosis was about 5 years ago persistent 150+/90ish monitored a lot for 6 months in spite of serious levels of fitness for 30 years and no other life style risk factors. My dad "gave" it to me as a present (along with the OA in my knees!) There was no way of increasing exercise or changing diet in any significant way. Started treatment with Telmisartan (Micardis) which is an ARB (Angiotensin Receptor blocker) rather than an ACE inhibitor. Since treatment have been continuously 120/80 and all my PBs have been set since treatment started so no negative effect at all.
Interestingly I discovered tonite that there is a secondary effect on muscle that in fact may be beneficial to exercise and has been suggested as a metabolism modifier that has some interest via WADA (though isn't on any lists). https://insights.ovid.com/crossref?an=0 ... 3000-00002
Lindsay
72yo 93kg
Sydney Australia
Forum Flyer
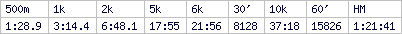
PBs (65y+) 1 min 349m, 500m 1:29.8, 1k 3:11.7 2k 6:47.4, 5km 18:07.9, 30' 7928m, 10k 37:57.2, 60' 15368m
72yo 93kg
Sydney Australia
Forum Flyer
PBs (65y+) 1 min 349m, 500m 1:29.8, 1k 3:11.7 2k 6:47.4, 5km 18:07.9, 30' 7928m, 10k 37:57.2, 60' 15368m
- DNA_Rower
- 1k Poster
- Posts: 160
- Joined: October 16th, 2011, 7:08 pm
- Location: Berlin, Germany
- Contact:
Re: Reduced blood pressure = reduced performance?
Thanks for the comments guys. This is useful input.
To provide some extra context:
I have been investigating this for about 1.5 years now, first in the UK with the NHS, now with the German health system. I have a home measuring device that I have been using consistently in that time, and have done several 24h tests with the device from the doctors (fun!). One interesting point is that my sleeping BP is in the normal range, but waking BP is too high (that does not automatically mean it is "stress" though).
I went on Ramipril, which is an ACE inhibitor, at first and went up to the maximum dose over a long period, and my BP was still too high. Added in a calcium antagonist - made no difference.
I got switched on to the triple combo drug, which immediately brought my BP down to a normal/optimal range. It was quite surprising after consistently being 14X/9X minimum to suddenly be getting 12X/7X. However - the effect on my erg timing was also immediate. The day after I changed medicine I went on the erg and struggled. After more or less progressing every week for the last two years (other than a couple of set backs earlier this year) I overnight lost about 10% stamina.
Last Thursday night I started to feel really faint and in the morning my BP was 110/57, which is way too low for me so I stopped taking the medicine and took an erg break.
BP is now back up to 138/78. Too high on the systolic but ok on the diastolic. I went back to the gym and did a SS 10k and I managed a 2:00 pace fine. Last week I struggled to get a 2:06 pace. It is a really dramatic change.
wrt to lifestyle etc thanks but I am sure my lifestyle is not to blame here. I'm 184cm and 80kg. It's a good weight for my height. I'm pretty active, cycling to work every day and erging 4-6 times a week. Diet is not too bad (for a Scotsman! No fried mars Bars!).
thanks but I am sure my lifestyle is not to blame here. I'm 184cm and 80kg. It's a good weight for my height. I'm pretty active, cycling to work every day and erging 4-6 times a week. Diet is not too bad (for a Scotsman! No fried mars Bars!).
I think, given this new medicine seems to work, I just have to find the dose that gets me to 120/80. Then I can start pulling in PBs again!
To provide some extra context:
I have been investigating this for about 1.5 years now, first in the UK with the NHS, now with the German health system. I have a home measuring device that I have been using consistently in that time, and have done several 24h tests with the device from the doctors (fun!). One interesting point is that my sleeping BP is in the normal range, but waking BP is too high (that does not automatically mean it is "stress" though).
I went on Ramipril, which is an ACE inhibitor, at first and went up to the maximum dose over a long period, and my BP was still too high. Added in a calcium antagonist - made no difference.
I got switched on to the triple combo drug, which immediately brought my BP down to a normal/optimal range. It was quite surprising after consistently being 14X/9X minimum to suddenly be getting 12X/7X. However - the effect on my erg timing was also immediate. The day after I changed medicine I went on the erg and struggled. After more or less progressing every week for the last two years (other than a couple of set backs earlier this year) I overnight lost about 10% stamina.
Last Thursday night I started to feel really faint and in the morning my BP was 110/57, which is way too low for me so I stopped taking the medicine and took an erg break.
BP is now back up to 138/78. Too high on the systolic but ok on the diastolic. I went back to the gym and did a SS 10k and I managed a 2:00 pace fine. Last week I struggled to get a 2:06 pace. It is a really dramatic change.
wrt to lifestyle etc
I think, given this new medicine seems to work, I just have to find the dose that gets me to 120/80. Then I can start pulling in PBs again!
A: 40; H: 184cm; W: 76kg.
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
- gregsmith01748
- 10k Poster
- Posts: 1359
- Joined: January 8th, 2010, 2:17 pm
- Location: Hopkinton, MA
Re: Reduced blood pressure = reduced performance?
Hi,
If one of the meds in your cocktail is a beta blocker, they have a well established effect on heart rate and impact on exercise performance.
https://www.ncbi.nlm.nih.gov/pubmed/2866577
Greg
If one of the meds in your cocktail is a beta blocker, they have a well established effect on heart rate and impact on exercise performance.
https://www.ncbi.nlm.nih.gov/pubmed/2866577
Greg
Greg
Age: 55 H: 182cm W: 90Kg

Age: 55 H: 182cm W: 90Kg

-
Brian Lancaster
- Paddler
- Posts: 46
- Joined: March 31st, 2009, 7:34 pm
- Location: Worthing West Sussex UK
Re: Reduced blood pressure = reduced performance?
In my opinion (as a past user) beta blockers should be banned. They dilate the arteries allowing easier passage of blood but they do nothing to limit the original condition. So if the problem is arterial cholesterol, there is no preventative effect. If the lifestyle of the user does not change then cholesterol deposition continues.
This is why the leaflets in the capsule boxes state that the user MUST NOT suddenly stop taking beta blockers. If a user has taken them for a significant period of time, then cholesterol build up will have continued (if no lifestyle changes have been made). Sudden stoppage will cause the dilated arteries to contract again and they will now be more severely restricted or possibly even blocked altogether. So a potentially dangerous or even fatal situation may be produced.
In my case, I found that cardiac output was limited so severely that even quite modest exercise was very tiring and unpleasant. My particular prescribed drug was Atenolol. I retired on medical grounds at 53 with a 'heart condition '. A specialist had prescribed the drug after halting a treadmill test that he put me through. I said , when he announced that he was going to stop the machine, that I was ok and could go faster. His response was that he could see from the monitor trace that my heart was labouring and insisted on stopping.
He showed me the monitor trace when I had got off the treadmill and pointed out a concave line that, with a healthy individual, should have been convex. It so happened that I knew exactly what he was talking about because one of the subjects that I lectured in was thermodynamics. In testing internal combustion engines in the lab I used to produce 'indicator diagrams'. These are diagrams of cylinder pressure in relation to piston position through the two stroke, four stroke, diesel etc. cycles. They are used to calculate engine efficiency. They are enclosed loops of a shape characteristic of the particular engine type. In general, the bigger the enclosed area of the Koop the more efficient the engine because that area represents the work done in the cycle.
In the trace from the heart monitor it is exactly the same and the concave line on mine was greatly reducing the loop area.
I returned to the same specialist after some months on beta blockers for a repeat of the treadmill test. This time the trace produced was an apparently 'much healthier' one of significantly larger area. The disastrous difference for me was that, in this case, I felt that I was dying and was desperate for the machine to be stopped. He said that he was now dubious about his recommendation of early retirement on medical grounds. I told him how awful I had felt during the test and managed to persuade him to stick with the recommendation. Fortunately for me, since medical retirement was funded by central rather than local government and, even more fortunately, since my college had too many senior staff, the Principal was happy to go along with the recommendation. I was retired with pension enhancement as if I were retiring at age sixty. Great.
However, the beta blockers were making my life miserable and despite 'what it said on the tin', I stopped using them. At least, off them, I could enjoy what time I had left a lot more. Several years later, quite by accident, I found a book in the library by an Amercan heart specialist, Dean Ornish. It was called 'Reversing Coronary Heart Disease'. I am not sure if it is still in print but I can assure you that IT WORKS. I followed its principles to the nth degree and eventually was able at age 65 to win BIRC in what was then a championship record time of 7:05.2.
I also went back to the same specialist and did the treadmill test now, twelve or so years later, without any drugs. He said that I now appeared to have no heart problems. I took the book to show him but he was not impressed.
So, if anyone reading this is taking beta blockers, I would recommend a lifestyle change and a weaning off them. In consultation with your GP of course. I am now eighty and feeling great. I have been fairly relaxed but not casual about lifestyle in the intervening years since being 65, until last August. With a new age category approaching, I decided once more to really go all out again in training and lifestyle.
I currently hold two World and one British record in my age category and I expect to rank at least in the top three at all events that I try on the C2 ranking site this season. My blood pressure is around 120/70 measured on the professional machine at my GP surgery. I find that it is important to fully relax for several minutes sitting at the machine before actually taking the reading. It is very easy to get readings higher than the minimum, fully relaxed, ones. These are the 'true' readings needed for proper accuracy if one is needing reassurance about blood pressure.
This is why the leaflets in the capsule boxes state that the user MUST NOT suddenly stop taking beta blockers. If a user has taken them for a significant period of time, then cholesterol build up will have continued (if no lifestyle changes have been made). Sudden stoppage will cause the dilated arteries to contract again and they will now be more severely restricted or possibly even blocked altogether. So a potentially dangerous or even fatal situation may be produced.
In my case, I found that cardiac output was limited so severely that even quite modest exercise was very tiring and unpleasant. My particular prescribed drug was Atenolol. I retired on medical grounds at 53 with a 'heart condition '. A specialist had prescribed the drug after halting a treadmill test that he put me through. I said , when he announced that he was going to stop the machine, that I was ok and could go faster. His response was that he could see from the monitor trace that my heart was labouring and insisted on stopping.
He showed me the monitor trace when I had got off the treadmill and pointed out a concave line that, with a healthy individual, should have been convex. It so happened that I knew exactly what he was talking about because one of the subjects that I lectured in was thermodynamics. In testing internal combustion engines in the lab I used to produce 'indicator diagrams'. These are diagrams of cylinder pressure in relation to piston position through the two stroke, four stroke, diesel etc. cycles. They are used to calculate engine efficiency. They are enclosed loops of a shape characteristic of the particular engine type. In general, the bigger the enclosed area of the Koop the more efficient the engine because that area represents the work done in the cycle.
In the trace from the heart monitor it is exactly the same and the concave line on mine was greatly reducing the loop area.
I returned to the same specialist after some months on beta blockers for a repeat of the treadmill test. This time the trace produced was an apparently 'much healthier' one of significantly larger area. The disastrous difference for me was that, in this case, I felt that I was dying and was desperate for the machine to be stopped. He said that he was now dubious about his recommendation of early retirement on medical grounds. I told him how awful I had felt during the test and managed to persuade him to stick with the recommendation. Fortunately for me, since medical retirement was funded by central rather than local government and, even more fortunately, since my college had too many senior staff, the Principal was happy to go along with the recommendation. I was retired with pension enhancement as if I were retiring at age sixty. Great.
However, the beta blockers were making my life miserable and despite 'what it said on the tin', I stopped using them. At least, off them, I could enjoy what time I had left a lot more. Several years later, quite by accident, I found a book in the library by an Amercan heart specialist, Dean Ornish. It was called 'Reversing Coronary Heart Disease'. I am not sure if it is still in print but I can assure you that IT WORKS. I followed its principles to the nth degree and eventually was able at age 65 to win BIRC in what was then a championship record time of 7:05.2.
I also went back to the same specialist and did the treadmill test now, twelve or so years later, without any drugs. He said that I now appeared to have no heart problems. I took the book to show him but he was not impressed.
So, if anyone reading this is taking beta blockers, I would recommend a lifestyle change and a weaning off them. In consultation with your GP of course. I am now eighty and feeling great. I have been fairly relaxed but not casual about lifestyle in the intervening years since being 65, until last August. With a new age category approaching, I decided once more to really go all out again in training and lifestyle.
I currently hold two World and one British record in my age category and I expect to rank at least in the top three at all events that I try on the C2 ranking site this season. My blood pressure is around 120/70 measured on the professional machine at my GP surgery. I find that it is important to fully relax for several minutes sitting at the machine before actually taking the reading. It is very easy to get readings higher than the minimum, fully relaxed, ones. These are the 'true' readings needed for proper accuracy if one is needing reassurance about blood pressure.
B.L.
Re: Reduced blood pressure = reduced performance?
Went to the Drs today to get a checkup for my license renewal. Turns out my bp is quite low. More so than usual. Doc wanted to know if i get dizzy spells etc. Nope.... but I did say I hadn't had much to drink today.... So they put it down to that.
Need to keep the fluids up
Need to keep the fluids up
Erik
61 yo from New Zealand
6'4 and 120kg
61 yo from New Zealand
6'4 and 120kg
- DNA_Rower
- 1k Poster
- Posts: 160
- Joined: October 16th, 2011, 7:08 pm
- Location: Berlin, Germany
- Contact:
Re: Reduced blood pressure = reduced performance?
Wow that was a very interesting post Brian. Thanks for sharing that information.
I had my cholesterol checked fairly recently and it was fine.
I'm not on a beta blocker. My triple combo pill is: olmesartan medoxomil + amlodipine + hydrochlorothiazide. So that is an angiotensin receptor blocker (as opposed to ACE inhibitor), a calcium channel blocker and a diuretic.
Basically my doctor told me to get a pill splitter, halve the dose and go from there. There are oodles of different dose combinations for this drug so it could take a while to find the one that lowers my BP but still allows me to train at maximal effort.
I am getting quite bored of running a pharmacological experiment on myself though!
I had my cholesterol checked fairly recently and it was fine.
I'm not on a beta blocker. My triple combo pill is: olmesartan medoxomil + amlodipine + hydrochlorothiazide. So that is an angiotensin receptor blocker (as opposed to ACE inhibitor), a calcium channel blocker and a diuretic.
Basically my doctor told me to get a pill splitter, halve the dose and go from there. There are oodles of different dose combinations for this drug so it could take a while to find the one that lowers my BP but still allows me to train at maximal effort.
I am getting quite bored of running a pharmacological experiment on myself though!
A: 40; H: 184cm; W: 76kg.
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
PBs: 2k 6:56.9; 6k 22:40.9 (all 2017/2018). 5k 18:28.9; 30min 8,005m; 10k 38:09.8 (2020)
Doing PP|Hate the heat
-
Brian Lancaster
- Paddler
- Posts: 46
- Joined: March 31st, 2009, 7:34 pm
- Location: Worthing West Sussex UK
Re: Reduced blood pressure = reduced performance?
I have also found that accepting a cholesterol reading as 'fine' from a GP is too simple. It may well be that your reading is good. I always ask for a printout of any blood test reading. This will state the correct scientific units rather than a broad brush plain number that GP's tend to state to patients whom they see as laymen. (Which the vast majority are).
There is no problem doing this, in fact GP's usually respond very favourably when a patient shows some more than rudimentary interest in his symptom analysis.
What started me on my current drive to maximise fitness (apart from starting at the bottom of the 80-89 category) was the results of an investigative blood test (March 12 th 2018) that produced one and a half pages of A4 printout from the hospital lab. The doctor had read this through and reported to me that all was well except for a Serum (CHOW 1220) cholesterol that was given as 5.5 mmol/litre. This was listed as 'Borderline/Satisfactory. The printout showed an acceptable range of 2.00-5.00 mmol/litre and stated the desirable level as < 4.8 mmol/litre.
What had caused me to ask for the test was an episode of prolonged shallow, very rapid heartbeat (175 b/m) on the exercise bike which did not stop when I stopped. I usually will go to 150 b/m under peak stress on a random load programme on the bike. I know when my heart goes 'off on one' like that. I can feel it in my neck. It is called paroxsysmal tachycardia and is quite common apparently. It normally resets quite abruptly a few seconds after stopping and then jumps to a very strong quite slow beat. This time it persisted fast for close to half an hour. (No pain or other adverse symptoms). So I reported to the GP who printed me a blood test request form which can be taken to the hospital and carried out on demand. She also arranged a lung function test with the nurse which was done a couple of days later. (Who says that the NHS is not working as it should? In my experience it has always been excellent.)
One thing that she said to me when I first saw her was that she could see signs of elevated cholesterol in the whites of my eyes while bp and lungs seemed fine. That set me immediately on the Mayo Clinic initial crash diet and by the time I saw her again for the blood test results I had lost nearly half a stone. She seemed impressed by the fact that I had acted immediately on her initial (and correct) cholesterol diagnosis. She said that she would arrange for me to undergo a heart stress test at the hospital. That appointment has still not come through but I am hoping to persuade the tester to make it really stressful as my fitness levels have improved massively with all this gym and erg work. I have a rigorous, proper food regime going too. I have lost twenty pounds since starting these regimes. I thought I was not that much overweight to start at six foot, 201 lbs but the health stats still put my bmi toward the high end of the healthy range.
One final observation about so called 'normal' bp readings. I have not researched this but have heard it said that what we class as normal is in fact quite high when compared to the bp of Africans in Africa. Presumably diet but possibly exercise related, I have heard that typical readings are likely to be 100/? Whether that is necessarily good, I don't know but our 'normal' may not be that great after all.
There is no problem doing this, in fact GP's usually respond very favourably when a patient shows some more than rudimentary interest in his symptom analysis.
What started me on my current drive to maximise fitness (apart from starting at the bottom of the 80-89 category) was the results of an investigative blood test (March 12 th 2018) that produced one and a half pages of A4 printout from the hospital lab. The doctor had read this through and reported to me that all was well except for a Serum (CHOW 1220) cholesterol that was given as 5.5 mmol/litre. This was listed as 'Borderline/Satisfactory. The printout showed an acceptable range of 2.00-5.00 mmol/litre and stated the desirable level as < 4.8 mmol/litre.
What had caused me to ask for the test was an episode of prolonged shallow, very rapid heartbeat (175 b/m) on the exercise bike which did not stop when I stopped. I usually will go to 150 b/m under peak stress on a random load programme on the bike. I know when my heart goes 'off on one' like that. I can feel it in my neck. It is called paroxsysmal tachycardia and is quite common apparently. It normally resets quite abruptly a few seconds after stopping and then jumps to a very strong quite slow beat. This time it persisted fast for close to half an hour. (No pain or other adverse symptoms). So I reported to the GP who printed me a blood test request form which can be taken to the hospital and carried out on demand. She also arranged a lung function test with the nurse which was done a couple of days later. (Who says that the NHS is not working as it should? In my experience it has always been excellent.)
One thing that she said to me when I first saw her was that she could see signs of elevated cholesterol in the whites of my eyes while bp and lungs seemed fine. That set me immediately on the Mayo Clinic initial crash diet and by the time I saw her again for the blood test results I had lost nearly half a stone. She seemed impressed by the fact that I had acted immediately on her initial (and correct) cholesterol diagnosis. She said that she would arrange for me to undergo a heart stress test at the hospital. That appointment has still not come through but I am hoping to persuade the tester to make it really stressful as my fitness levels have improved massively with all this gym and erg work. I have a rigorous, proper food regime going too. I have lost twenty pounds since starting these regimes. I thought I was not that much overweight to start at six foot, 201 lbs but the health stats still put my bmi toward the high end of the healthy range.
One final observation about so called 'normal' bp readings. I have not researched this but have heard it said that what we class as normal is in fact quite high when compared to the bp of Africans in Africa. Presumably diet but possibly exercise related, I have heard that typical readings are likely to be 100/? Whether that is necessarily good, I don't know but our 'normal' may not be that great after all.
B.L.